
The COVID-19 pandemic drastically affected the quality of life in Texas nursing facilities
The COVID-19 pandemic has been devastating for long-term care facilities in Texas and nationwide. Existing medical vulnerabilities, living in close quarters and experiencing a lack of effectively managed infection control protocols made residents of nursing homes and assisted living facilities particularly susceptible to the virus. Long-term care residents comprise approximately 15% of all COVID-19 deaths in the United States, according to CDC data.(1)
Additionally, facility staff members were also vulnerable and contracted the virus at high rates, exacerbating the existing staffing crisis in many facilities, and leaving residents without regular assistance for daily living activities such as eating, hygiene, and recreation. Policies meant to halt the spread of COVID-19 also greatly limited or even completely halted visitation, leaving residents isolated from family all while staffing shortages often left residents isolated and confined within.(2)
Fully understanding the impact of the pandemic on residents of long-term care facilities will take some time. In collaboration with the Long Term Care Ombudsman, Texas Appleseed conducted an initial review of information from the Minimum Data Set, a compilation of various health indicators collected by the federal government, seeking to understand the overall impact of the pandemic on residents’ health, well-being, and quality of life.(3)
It is difficult to draw any specific conclusions from physical health indicators, in part because COVID-19 so dramatically impacted resident health in most nursing facilities. Most of the indicators we reviewed, such as the amount of assistance residents required for basic activities like eating and toilet use, remained relatively stable. More concerning, however, was a notable change in the number of residents that experienced significant, unplanned weight loss (>5% weight loss in 30 days or >10% weight loss in 180 days). As shown in Figure 1, the percentage of residents with unexpected weight loss increased from 4.3% in Q4 2019 (pre-pandemic) to 7.09% in Q3 2020, a 65% increase.
Figure 1. Unplanned Weight Loss in Texas Nursing Facilities, 2017-Q2 2021

Unplanned weight loss contrasts to other observed physical health indicators in its relationship with staffing and mental health. Overtaxed staff may struggle to get residents their meals with regularity, and the isolation experienced by residents during the pandemic-associated lockdowns may have contributed to reduced appetite or desire to eat, in turn contributing to weight loss. The currently available data are primarily descriptive, but these correlations will likely be explored by researchers for years to come.
Mental health indicators showed the most profoundly negative effect of the pandemic and the weakest recovery in the first two quarters of 2021. Figures 2-4 show the sudden and dramatic increase in the prevalence of anxiety disorder, depression, and poor mental well-being with the onset of the pandemic and associated lockdowns.
Figure 2. Prevalence of Diagnosed Anxiety Disorder in Texas Nursing Facilities, 2017-Q2 2021
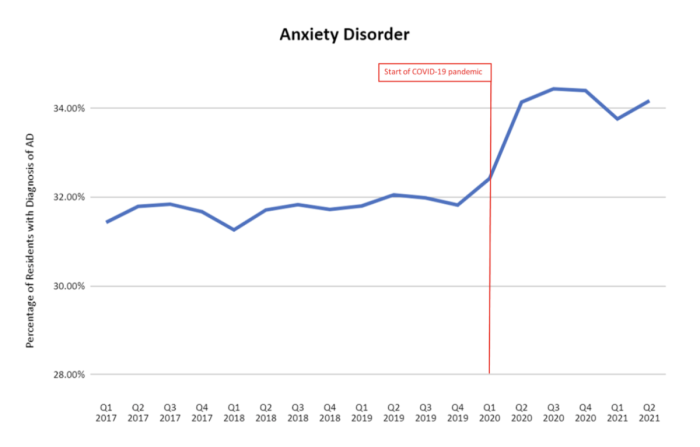
Figure 3. Prevalence of Diagnosed Depression in Texas Nursing Facilities, 2017-Q2 2021
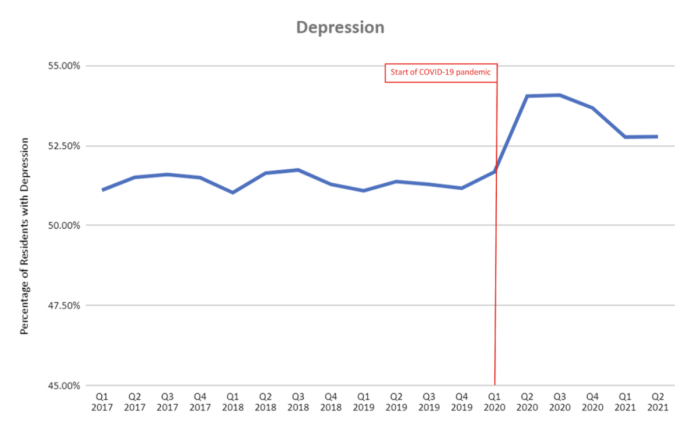
Figure 4. Percentage of Texas Nursing Facility Residents Feeling Down, Depressed or Hopeless, 2017-Q2 2021
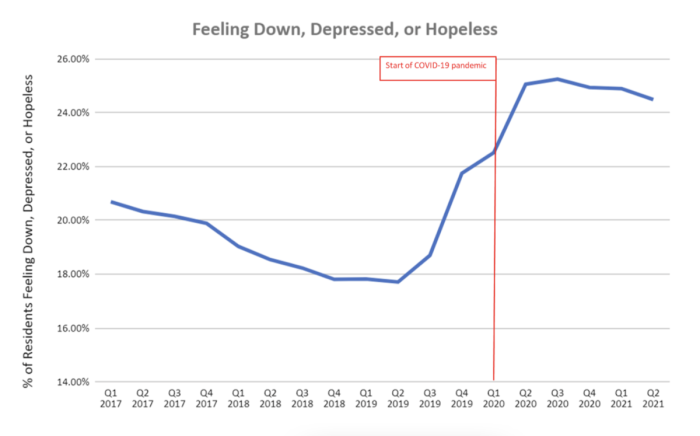
The conditions residents of long-term care facilities faced as a result of measures taken to prevent the spread of COVID-19 likely took a toll. Generally, only certain staff members, medical professionals, and other essential service providers could enter a nursing facility — not family members. Worse, a perpetual shortage of these staff members forced residents to contend not only with separation from their loved ones, but also from each other and their regular staff caregivers. Recognizing the devastating consequences of this separation and responding to an outcry from family caregivers statewide, the Legislature passed Senate Bill 25 and Senate Joint Resolution 19, which established residents’ right to an essential caregiver who cannot be denied access to a nursing facility in the Texas Constitution. Voters overwhelmingly approved the measure in November 2021.(4)
In contrast to the weight loss data and other physical indicators, these mental health indicators also show relatively weak recovery in Q1 and Q2 of 2021, a concerning trend, especially when combined with the alarmingly high prevalence of mental health conditions in long-term care facilities. Pre-pandemic, more than half of nursing facility residents had a depression diagnosis, indicating a strong need for better mental health services for persons living in long-term care facilities. Expanding access to these services will be essential.
Texas Appleseed envisions an approach to long-term care that reflects the preferences and vigorously protects the rights of elderly Texans and people with disabilities. As the role of the pandemic and its effects on our day-to-day lives continues to evolve, we will continue to monitor these data and pursue evidence-based policy solutions to improve mental health services in long-term care facilities, as well as interventions that preserve and protect the overall health and well-being of elder Texans.
(1)COVID-19 Nursing Home Data, from Centers for Medicare and Medicaid Services.
(2) Guidance for Infection Control and Prevention of Coronavirus Disease 2019 (COVID-19) in Nursing Homes, from Centers for Disease Control & Prevention.
(3)Minimum Data Set, Center for Medicare and Medicaid Services.
(4)Texas voters back long-term care residents’ right to in-person visits, from KERA News, November 3, 2021.